What is Platelet Rich Plasma (PRP)?
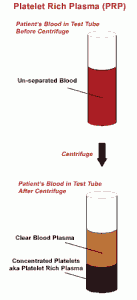
PRP refers to a concentrate of platelets in plasma that is higher than that of normal circulating platelets in the body. Beyond this concept, however, there is considerable variation in its definition.
Platelets have a vital role in the healing of injured tissues. The alpha granules of platelets contain growth factors which result in various biological effects. However, variations in individuals and differences in preparation methods can affects the absolute and relative concentrations of these different factors in PRP, which could account for differences in clinical outcome.
The release of these factors can be rapidly triggered by platelet activators thrombin and calcium. This results in the formation of a gel which can be used in open surgery but is impractical for injection. More gradual activation of platelets is also possible through exposure to damaged collagen, which attracts platelets through cytokine for PRP to be administered without pre-activation into damaged tissues.
Experimental and benefit of PRP
The biological effects of PRP and the various platelet-derived factors have been the subject of a considerable amount of laboratory-based research. Studies in animals have shown that for ligament repairs, PRP could result in improved maximal ligament load and linear stiffness. For tendon repairs, the addition of PRP resulted in significantly stronger healing, compared with the control side. Various positive effects on cartilage synthesis have also been seen with PRP and its factors. PRP has also shown potential to modulate inflammation.
Most recent reviews on PRP have concluded that there is a sound scientific basis for its use in soft tissue injuries, but have highlighted the lack of robust clinical data. Truly randomized, placebo-controlled, blinded trials are currently lacking. Clinical reports so far tend to be summations of experiences in groups of patients, or comparative studies against a more established treatment method. It has been reported that muscle tears heal twice as fast with PRP. Other clinical reports in medical press or conference proceedings have reported positive effects of PRP in tennis elbow, Achilles tendonitis, ankle sprains and osteoarthritis. While there appears to be overall support for PRP in soft tissue and wound healing, the benefit of PRP for bone repair and bone graft healing remains controversial.
Clinical Application in Sports and Musculoskeletal Medicine
A vast majority of sport and exercise related injuries involve soft tissue and are not severe enough to warrant surgery. Such injuries would usually heal on their own over time. A typical muscle strain, for example, would go through phases of homeostasis, inflammation, regeneration (replacement with original tissue) and repair (scar tissue). The management of such injuries typically involves management of inflammation and pain, combined with physiotherapy to address related issues such as spasm, muscle imbalances or joint stiffness which may have predisposed the patient to the injury. Essentially, the injured tissue is left to heal on its own, as determined by the body’s natural pace of healing.
PRP, with its potential to quicken healing, appears to be an attractive option for sportsmen or exercisers wishing to minimize injury downtime from both acute as well as overuse injuries. With an increasing numbers of adults and mid-lifers adopting exercise as a lifelong habit, degenerative and overuse injuries are becoming increasingly commonplace. PRP treatment once again presents itself as being a potential part of the solution for such injuries.
Current uses for PRP in Sports Medicine include:
- Chronic Insertional or Intrasubstance tendinopathy with or without tear, Eg. Tennis Elbow, Patellar tendinosis, Insertional Achilles Tendinosis, Plantar Faciitis, Rotator Cuff tendinosis.
- Ligament tears, eg. Medial Collateral Ligament (MCL) of the knee, Ankle ligament sprains
- Post-surgical augmentation of soft tissue healing, eg. Following surgical tendon repairs in tendo-achilles or rotator cuff, meniscus repair, or cartilage surgery in degenerative joint disease.
- Cartilage degeneration and early stages of osteoarthritis of the knee, ankle and other joints.
- Acute muscle tears eg. Myoseptal tears of the calf of hamstring
Need consultation? Our professional orthopaedic specialist, Dr. Kevin Yip, has more than 20 years experience. Be assured that you will be receiving professional treatments that suit your needs.
Call +65 6471 2691